Department of Medical Education and General Medicine, Graduate School of Medicine, Hokkaido University
Makoto Takahashi, M.D., Ph.D.Social
Medicine
- Education:
-
- 1997-2001
- Tokyo Med& Dent Univ Graduate School of Medicine Department of Orthopaedic Surgery
- 1986-1992
- Tokyo Med& Dent Univ School of Medicine
- Academic & Professional Experience
-
- 1992-1993
- Tokyo Med & Dent Univ Hospital Orthopaedic surgery Resident
- 1993-1993
- Omiya Redcross Hospital Anesthesiology Resident
- 1994-1994
- Nakano General Hospital Orthopaedic surgery Resident
- 1994-1994
- Kudanzaka Hospital Orthopaedic surgery Resident
- 1995-1997
- Suwa Central Hospital Orthopaedic surgery Resident
- 2001-2002
- Saiseikai Kawaguchi General Hospital Orthopaedic surgery Fellow
- 2002-2003
- Kudanzaka Hospital Orthopaedic surgery Fellow
- 2003-2003
- Tokyo Med & Dent Univ Hospital Orthopaedic surgery Fellow
- 2003-2004
- Tokyo Med & Dent Univ Graduate School of Med & Dent sciences Orthopaedic and Spinal Surgery Assistant Professor
- 2004-2007
- Tokyo Med & Dent Univ Graduate School of Med & Dent sciences Orthopaedic surgery Assistant Professor
- 2007-2009
- Suwa Central Hospital Orthopaedic surgery Dept Chairperson
- 2009-2019
- Tokyo Med & Dent Univ Graduate School of Med & Dent sciences Medical Education Research & Development Lecturer
- 2013-2019
- Tokyo Medical and Dental University University Hospital of Medicine
- 2014-2019
- Tokyo Medical and Dental University Hospital of Medicine
- 2019-Today
- Hokkaido Univ Faculty of Medicine Center for Medical Education and International Relations Professor
- 2019-Today
- Center for Medical Education and International Relations at the Faculty of Medicine, Hokkaido University Deputy General Director
Using the new EPOC2 online clinical education evaluation system as a career development portfolio

While involved in medical treatment, research, and guidance for young people as an experienced orthopedic surgeon, Professor Makoto Takahashi, who is familiar with medical education, has actively assisted national administrative measures regarding medical education. Since taking office as the professor of the Department of Medical Education and General Medicine in 2019, and while also managing the department, he has been involved in the development of the EPOC2 online postgraduate clinical education evaluation system and the OSCE medical common achievement tests for medical students, and has engaged in research and development toward the realization of seamless medical education, from clinical clerkship for medical students to postgraduate clinical training and subsequent specialty training.
Clinical training, which is an essential requirement for clinicians, began shortly after the Second World War with a postgraduate internship system in which interns would spend a year rotating around individual medical fields. Under the subsequent Medical Practitioners Act amendment, the internship system after graduation was abolished in 1968, and the old clinical training system started. In 2004, a new postgraduate medical training system was launched in response to the ordinance [1] on clinical training of the Ministry of Health, Labour and Welfare (MHLW), and it has been reviewed every five years since then.
In line with the start of this new postgraduate medical training system, efforts were made to develop a system to evaluate and certify the skills of residents according to the training items (attainment targets) specified by the ministry ordinance, in categories that residents should experience in clinical training such as “physical examination, test, procedure” and “symptom, pathophysiology, disorder.” As a result, the first EPOC (Evaluation System of Postgraduate Clinical Training), a system that allows faculty and medical staff who evaluate residents to input evaluation details on a PC, was born in 2004.
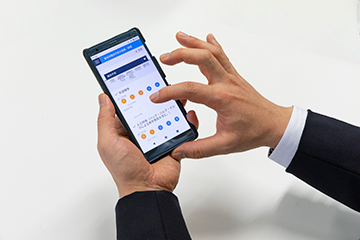
Professor Takahashi has been involved in the development of EPOC2, a renewed version of EPOC, since 2016. The goals of the renewal were as follows: 1. Easy input; 2. New evaluation form and 360-degree feedback; 3. Portfolio function; and 4. Possible future link to student/specialized training. Professor Takahashi says, “We have reviewed the evaluation items from the perspective of what the evaluation is for and what kind of evaluation is appropriate, and improved usability so that users can enter data by simply tapping the screen of their smartphone.”
He added, “In response to feedback from the teaching hospital that the evaluation items were insufficient, we have changed the scale of the evaluation on physical examination from the simple a. Sufficiently able; b. Able; and c. Effort required, to a style that specifically defines evaluation criteria, as follows: 1. Can do under the direct supervision of faculty; 2. Can do in a situation where faculty can respond immediately; 3. Can do almost alone; and 4. Can instruct junior fellows.”
“The major improvement in EPOC2 is that residents can freely write a review of training, participation in seminars and study sessions, academic activities and various other leaning records in the comment field,” Professor Takahashi continues. “EPOC started as a tool that supports training evaluation recording work set by MHLW. However, I would like it to be a system for residents. I hope that residents will use EPOC2 as a portfolio for career development throughout their lives and feel their own development in detail.” (Figure 1).
Although there is no legal provision for the evaluation recording tool, Professor Takahashi is proud that “90% of teaching hospitals now use EPOC2.” He says, “In response to the requests of many users, we are now improving the functions that most urgently require improvement.”
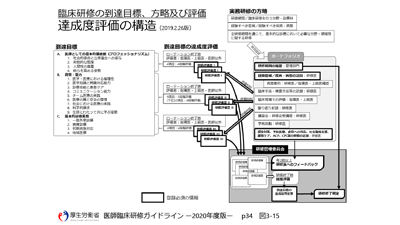
Underlying the EPOC renewal is the concept of “reforms for the seamless training of doctors,” which is being jointly promoted by the Ministry of Education, Culture, Sports, Science and Technology (MEXT) and MHLW. To eliminate duplication and blanks in training and improve the qualifications of doctors by unifying the process from undergraduate clinical clerkship in medical school under the jurisdiction of MEXT to postgraduate clinical training under the jurisdiction of MHLW and subsequent specialty training, and providing medical education for developing clinicians seamlessly and continuously, both ministries have shared information and exchanged personnel so that there is no policy conflict with each other.
Under that concept and as a research collaborator of MHLW’s adopted subject, “Study for Formulating Support Measures for Seamless Undergraduate and Postgraduate Medical Education Utilizing ICT – Construction of a Seamless Evaluation System Utilizing ICT,” Professor Takahashi has promoted the research and development of EPOC2, which allows users to consistently record the evaluation of all undergraduate and postgraduate training with mobile terminals. He has also been involved in the development of the OSCE medical common achievement tests, which medical students take around the time of clinical clerkship.
Even medical students need to have completed a certain level of study, including how to interact with patients.
OSCE (Objective Structured Clinical Examination) is a practical examination common to all medical schools nationwide. As clinical training (which is the latter-half curriculum of medical school) was changed from the conventional observation type to clinical clerkship based on the Model Core Curriculum for Medical Education established by MEXT in 2001, OSCE started in 2005 with the aim of evaluating whether medical students have the skills and attitudes to confidently engage in clinical clerkship that involves medical practice (Pre-Clinical Clerkship OSCE (Pre-CC OSCE)), and whether they are ready to participate in clinical training after graduating from medical school (Post-Clinical Clerkship OSCE (Post-CC OSCE), which started in 2020).
Professor Takahashi says, “The item ‘treat a joint’ was added to the evaluation items of the OSCE examination section about five years ago, when I also joined the effort as an orthopedic specialist. At that time, the so-called medical interview, in which doctors ask patients about their medical condition and history, was often criticized as ‘three-minute medical treatment.’ A patient group said that doctors should build relationships from the first time they talk to patients in an outpatient setting and that efficient treatment can only be achieved if a relationship of trust is established between them. Therefore, before talking to patients, even students need to have completed a certain level of study, including how to interact with patients.”
“Since I was a teenager, I've always liked teaching people and having fun with many people, so the profession I wanted to be was a doctor or a school teacher. I have always loved sports, so I went on to orthopedics, where I enjoyed interacting with young patients and residents and became interested in medical education,” Professor Takahashi says.

“When I provided medical treatment for patients with spinal issues in the outpatient department of the hospital where I used to work, I took more time than other doctors. It took a while for me to listen to the stories of elderly patients. I wanted to properly deal with the patients who managed to come to the outpatient department despite their pain.”
When asked about the medical care that will be required in the future and the qualities that doctors need in light of the current situation surrounding today’s medical practice, such as the ever-increasing knowledge of medical care and medicine, the evolution of technology through AI and ICT, the declining birthrate and aging population, and the declining population, the professor says, “Knowledge that has been memorized so far can be supplemented by searching the Internet. Literacy that makes full use of technologies such as smartphones and AI, which are the sources of knowledge, will be required from now on. The composition of the diseases to be treated changes as society is aging. Infectious and contagious diseases prevailed after the Second World War. When they settled down, cancer treatment became a priority issue, and lifestyle-related diseases became a problem in the longevity society after that. In the future super-aging society, I think that the weight of terminal care will increase.”
In the Department of Medical Education and General Medicine, the Professor says they will continue to develop teaching methods and materials as well as evaluation systems related to various types of training. “We also plan to undertake various studies on medical education, including those on the learning behavior of medical students and career selection of doctors,” he adds. “Many faculty members are also active in research on COVID-19 at Hokkaido University. First-class researchers are close to students and they can collaborate with various other faculties. This educational environment is ideal for medical students.”
[1] ^ The old clinical training system, whose main purpose was on-the-job training for residents who had joined a clinical department, was reviewed in the Medical Practitioners Act amendment in 2000 based on MHLW’s basic philosophy that clinical training “should allow residents to acquire basic medical abilities to properly deal with injuries and illnesses which they frequently encounter in general medical care.” As a result, a new postgraduate medical training system was launched to allow residents to develop comprehensive medical skills before joining a clinical department, and the training, which used to be the obligation to make efforts, has become mandatory for two years after graduation.
(Interviewed in December 2020)
Get tips for studying abroad, presenting at international conferences, and writing papers in English at medical English seminars
The Medical English Education Division of the Center for Medical Education and International Relations at the Faculty of Medicine, where Professor Takahashi serves as the deputy general director of the center, holds medical English seminars using Zoom for all students and faculty members on campus.
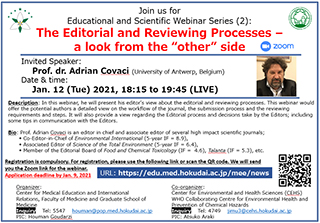
In academic 2019, basic seminars that are indispensable to the daily life of doctors were held, such as “Read English Papers,” “Participate in International Conferences,” “Give a Tour of the Hospital in English,” and “Explain Medicines in English.” In academic 2020, in-depth seminars were successfully held to provide useful information for students and researchers who are interested in studying abroad throughout the university. The seminars included “How to Win the Excellence Award in an English Poster Presentation at an International Conference” and “How to Write a Personal Statement in English and How to Build a Network” by Associate Professor Takayuki Oshimi (International University of Health and Welfare), who is a director of the Japan Society for Medical English Education, as well as “Recommendations to authors for writing interesting research articles” and “The Editorial and Reviewing Processes - a look from the “other” side” by Prof. Dr. Adorian Covaci of the University of Antwerp, Belgium.
Information on seminars in 2021 will also be available on the web as needed.