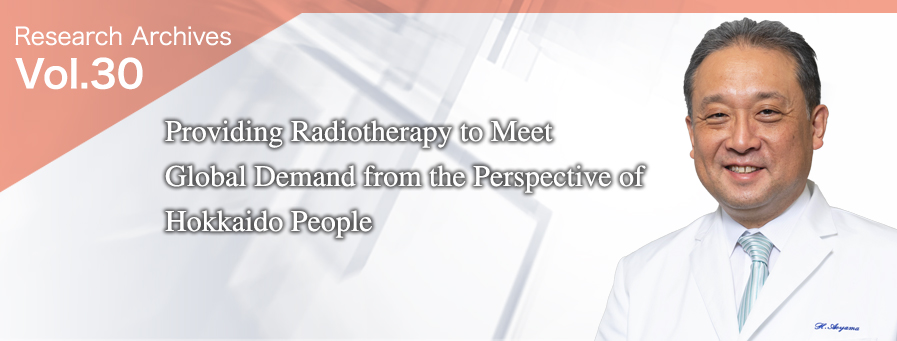
Department of Radiation Oncology, Graduate School of Medicine, Hokkaido University
Hidefumi Aoyama, M.D., Ph.D. Internal
Medicine
- Current Position:
-
Professor and Chair
Department of Radiation Oncology,
Hokkaido University Faculty of Medicine, Sapporo, Japan
- Education:
-
- 1988-1994
- Hokkaido University School of Medicine, M.D.
- 1998-2002
- Hokkaido University Graduate School of Medicine, Ph.D.
- Teaching Appointments:
-
- 1994-1996
- Resident, Sapporo City General Hospital
- 1996-1998
- Resident of Radiology and Radiation Oncology, Hokkaido University Hospital
- 2002-2007
- Assistant Professor, Department of Radiation Oncology, Hokkaido University Hospital
- 2007-2008
- Lecture, Department of Radiology, Hokkaido University Graduate School of Medicine
- 2008-2010
- Associate Professor, Department of Radiology, Hokkaido University Graduate School of Medicine
- 2010-2019
- Professor and Chair, Department of Radiology and Radiation Oncology, Niigata University Graduate School of Medical and Dental Sciences
- 2019-
- Professor and Chair, Department of Radiation Oncology, Hokkaido University Faculty of Medicine
Maintaining a balance between tumor control and cognitive preservation for treatment suitable for each patient

Radiotherapy is one of the three major cancer treatments along with surgery and chemotherapy using anticancer drugs, and it shrinks and kills cancer cells by irradiating the affected area with radiation such as X-rays or proton beams. Since 2019, Professor Hidefumi Aoyama has led the Department of Radiation Oncology (Radiation Oncology, Hokkaido University Hospital), which has been constantly developing advanced radiotherapy since its inception in 1947.
Professor Aoyama has faced many research issues as a leader in the treatment of brain tumors, especially metastatic brain tumors, which are difficult to handle. “The standard treatment for metastatic brain tumors used to be whole-brain radiotherapy (WBRT), with which the entire head is irradiated,” Professor Aoyama says. “In the 1990s, however, advances in computer technology made it possible to capture tumors in three-dimensional images, and the technology of stereotactic radiosurgery (SRS), which makes the irradiation target as small as possible, has been developed.”
With the evolution of technology, SRS, which was initially an auxiliary treatment for WBRT, has independently been conducted. Professor Aoyama has taken the lead in conducting multi‐institutional clinical trials and clarified the effect of treating metastatic brain tumors with SRS alone. After the research results were published in 2006 in JAMA (Journal of the American Medical Association), which is one of the world’s top medical journals, treatment with SRS alone became the global standard.
One of the reasons why treatment with SRS alone became the global standard is that cognitive decline was pointed out as a late effect of WBRT. However, with the widespread use of SRS alone, the frequent recurrence of intracranial tumors became a problem.
Then, to search an irradiation method that does not cause cognitive decline and does not interfere with recurrence control, Professor Aoyama started to create an international common language (index) for quantitatively evaluating cognitive function in 2008.
He collaborated with the Department of Psychiatry to create a Japanese version of the cognitive function test used in the United States. At Niigata University, where he took the post of professor in 2010, he started research on the international standard cognitive function evaluation index and therapeutic efficacy in collaboration with the US-led research group RANO (Response Assessment in Neuro-Oncology) and completed the evaluation index in 2019.
As a result of research, Professor Aoyama says, “It cannot be said that cognitive decline is caused solely by WBRT. Patients with a poor performance status develop cognitive decline naturally. If the tumor in the head is not controlled, it will also impair cognitive function, so tumor control is also important.”
Professor Aoyama also started studying a method of combining SRS, which intensively applies pinpoint radiation to patients with metastatic brain tumors, and WBRT, which applies radiation widely and thinly, and in 2015, he revealed in JAMA Oncology that there is a group of patients whose survival rate may increase by adding WBRT to SRS (Figure 1).
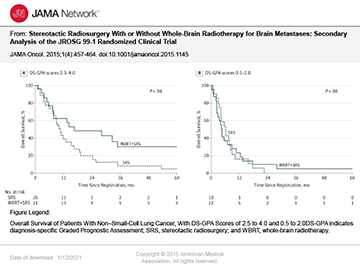
In 2020, Professor Aoyama conducted research on predictive indicators for prognosis after the treatment of metastatic brain tumors with other overseas research groups. “The criteria for the selection of treatment suitable for each patient were set, and based on the index, the Committee of Neuro-Oncology (chairperson: Professor Aoyama) of the Japanese Radiation Oncology Study Group (JROSG) takes the lead in research on optimization of whole-brain irradiation dosage to maintain a balance between tumor control and cognitive preservation. The combination of optimal radiotherapy with surgery, chemotherapy and drug therapy makes it possible to provide the most effective personalized treatment for individual patients,” he says.
Professor Aoyama believes in providing medical care to meet global demand from the perspective of Hokkaido people. “I have always wondered if medical care provided on the Hokkaido scale in terms of population density, land area, travel distance and the number of hospitals can become the world standard. There are only a few cities in the world that are comparable to the size of Tokyo, so I wonder if Hokkaido can be the average. I am working on research with the idea that the global treatment standard is based on that of Hokkaido.”
The gateway to the development of radiotherapists is to show medical students the appeal of radiology

“The Department of Radiation Oncology deals with cancer throughout the body. Members of the department are devoting themselves to research with their own research themes in collaboration with doctors in other fields, such as Neurosurgery, Gastroenterology and Hepatology, Gastroenterological Surgery, and Pediatrics. Individual faculty members specialize in different organs, and senior residents in and after their third year in the department switch their focus of care every few months so as not to create areas of weakness. Graduate students and senior residents receive the guidance of mentors according to their research theme and regularly report on the progress of their research at research meetings and other events.”
In the department, where almost all of the students go on to graduate school, first-year doctoral students Dr. Manami Otsuka and Dr. Yoshihiro Fujita have embarked on research to improve cancer therapy using radiation. According to Dr. Otsuka, who studies the treatment of head and neck cancer using proton beams, “The department has a system in place to concentrate on research. We learn how to read papers, make presentations, compile statistics, and so on at research meetings, and work on research while having discussions with each other.”
Meanwhile, Dr. Fujita says, “I was attracted to the sound of the futuristic phrase of ‘treating cancer with beams’ and aimed to become a radiotherapist.” He is now working on research to improve treatment results by visualizing the spread of tumors using apparent diffusion coefficient (ADC) taken from MRI images and irradiating them intensely.
“The appeal of radiotherapy is that it can be performed without cutting the affected area, which means less burden on patients. Once the standard treatment is decided, it can be applied to most patients, so there is no difference in treatment between individual doctors,” Professor Aoyama says. “As a result, the overall level of treatment is increased. It is possible to run a simulation before treatment, which is another advantage. We make several treatment plans and select the best one from them. It may be encouraging for doctors who are not good at making prompt decisions to have time for confirmation as a step before irradiation. The appeal of radiology in terms of research is that it involves all organs. From the perspective of radiotherapy, we can smoothly enter research in any area.”
“‘Study more’ is a common phrase for students,” Professor Aoyama says with a laugh. “I feel that there are many aspects of radiology that are not understood by medical students. Compared with Europe and the United States, where there are many radiotherapy facilities and therapists, in Japan, there are fewer medical staff members engaged in radiotherapy although capital investment is made. As a result, radiotherapy tends to become dysfunctional in Japan. Most of the current issues in radiotherapy can be solved if there are ‘people.’ I consider that the gateway to human resource development is to show medical students the appeal of radiology. The aim is a department chosen by students and residents for its future potential, where they can make a leap forward.”
[1] ^ The Department of Radiation Oncology, Hokkaido University Hospital has three X-ray radiotherapy systems, developed by the former Professor Hiroki Shirato, that have real-time tumor-tracking radiotherapy systems that enable pinpoint irradiation to moving organs, as well as one brachytherapy system used for cervical cancer treatment and one real-time tumor-tracking proton beam therapy system, allowing doctors to deal with cancer in all organs.
(Interviewed in December 2020)
“Turn misfortune into fortune” – online networking

“It’s a pity that we have been unable to do JINPA (Hokkaido University's popular Genghis Khan barbecue party) because of the COVID-19 pandemic after the department was launched, but there are also events that have turned misfortune into fortune,” Professor Aoyama says.
One of them is the online extended medical conference, which was held for the first time on December 10 and connected related hospitals all over Hokkaido. Initially, attendees had planned to meet in Sapporo, but the conference was held online as a measure against COVID-19. “It went unexpectedly well, so we would like to hold it about once every two months to create a sense of unity. Not everyone can visit Sapporo from all over Hokkaido, but the use of an online service makes it possible to involve more people all over Hokkaido,” the professor says. On this day, in addition to sharing information on academic conference fees, abstract registration, medical fee revision and other matters, there were also consultations from doctors in local cities regarding the introduction of special treatment equipment. Professor Aoyama says, “I am glad that we could exchange opinions.”
The Public Lecture by the Faculty of Medicine, Hokkaido University, entitled 北大医・市民公開講座「北海道で安心してがん治療を受けるために」“To Receive Cancer Treatment with Peace of Mind in Hokkaido,” will be available on YouTube every day from February 16 (Tue.) to 24 (Wed.). “As a result of web delivery as a measure against COVID-19, it has become possible to provide information to many people,” Professor Aoyama says. “Anyone can watch the easy-to-understand lectures about the latest medical treatment and advanced research by cancer treatment professionals and cancer researchers from medical universities in Hokkaido, on a personal computer or smartphone. They will also be available for on-demand viewing after the period.”
- 「北大医・市民公開講座」YouTubeチャンネル
“Public Lecture by the Faculty of Medicine, Hokkaido University” YouTube channel - 告知動画および ポスター動画
Announcement and poster videos - 北海道がんプロ・北大医・市民公開講座ってなに?
What is the Public Lecture by the Faculty of Medicine, Hokkaido University?